Malaysia's dialysis rates soar 600% since 1980s, projected to double by 2040
October 16, 2025
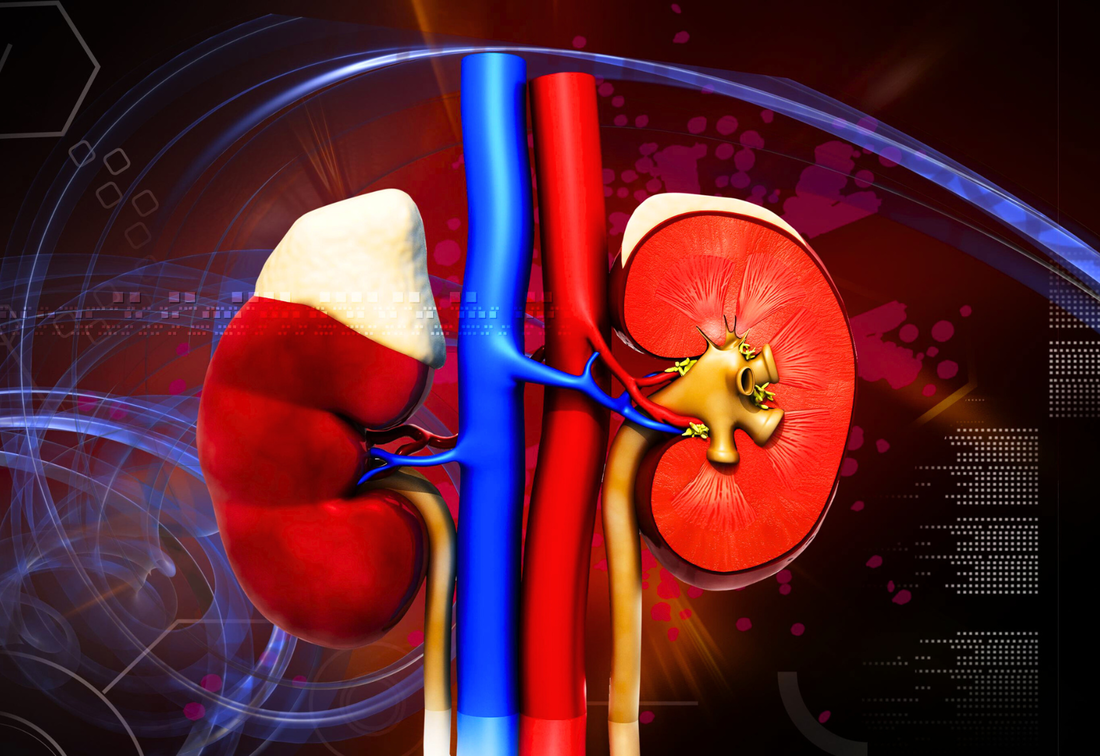
Kidney care in Malaysia has undergone significant evolution since its inception in the 1970s, marked by close collaboration between government, NGOs, and private sectors. The first hemodialysis unit was established at Kuala Lumpur General Hospital (HKL) in 1969, followed by the country's first kidney transplant in the 1970s. The peritoneal dialysis program began at University Hospital in 1981, marking five decades of kidney care development in Malaysia. Despite these successes, the system continues to face challenges including late referrals, increasing dialysis patients annually, low transplant rates, and significant financial stress.
Rising incidence and changing demographics The incidence of Chronic Kidney Disease (CKD) is increasing, primarily driven by diabetes and hypertension. As of 2024, approximately 85% of end-stage kidney disease cases are attributed to these two non-communicable diseases. Genetic kidney diseases are gaining recognition as an important factor, with Professor Lim Soo Kun noting that many genetic conditions remain undiagnosed due to limited genetic testing. The National Health and Wellbeing Survey reported a diabetes prevalence of 15.6% in 2023, which has consistently remained above 10% since tracking began, reaching as high as 18% in 2019. These insights were shared by Professor Lim at the National Kidney Foundation's 18th Annual Dialysis Conference - Innovate, Elevate, Transform, during his address on the "Kidney care burden in Malaysia: A journey through past challenges." Alarming projections and treatment statistics Malaysia has witnessed a dramatic increase in dialysis treatment rates, from 50 per million population in the 1980s to 300 per million population in 2024. Professor Lim warns that without drastic intervention, end-stage kidney disease cases could surge to 105,000 by 2040, up from over 53,000 dialysis patients in 2024. The demographic shift shows the highest growth among patients aged 55-64 and those 65 and older, presenting additional challenges as older patients typically have more comorbidities and increased frailty. Malaysia now ranks among the top 10 countries globally for new dialysis patients per million population, contrasting with European countries showing negative growth rates. Healthcare system and policy challenges Malaysia's current funding model presents significant challenges, with 60% of patients dialyzing in private centers while the Ministry of Health provides 50% of funding. The Social Security Organization (SOCSO) supports 25% of patients, with plans to increase the maximum hemodialysis treatment rate to RM170 per session in 2026, up from RM150. Less than 10% of patients self-fund their treatment, while only 2% rely solely on NGOs and charity. Professor Lim advocates for transitioning to a bundled payment system, similar to other countries, which would cover all aspects of dialysis treatment in a single comprehensive package. Geographic and resource disparities Significant regional disparities exist in dialysis access across Malaysia. While the national average dialysis treatment rate is 1,006 per million population, states like Perlis, Kelantan, Pahang, and Selangor fall below this figure, with Sabah having the lowest rate. East Malaysia generally has less access compared to West Malaysia, and the East Coast has fewer resources than the West Coast. The proportion of NGO dialysis centers has increased from one-third in 2004 to 50% currently, reflecting financial constraints and competition for qualified nurses who often move to private centers offering better pay. Workforce shortages and treatment limitations Malaysia faces significant workforce shortages in nephrology care. The country has approximately 270-300 practicing nephrologists, translating to 18 per million population, considerably lower than Taiwan (65 per million) and Japan (75 per million). Despite training more than 20 nephrologists annually, the numbers remain insufficient. The last recorded data on dialysis nurses in 2011 showed 62 per million population, a figure that requires updating. The majority of patients receive center-based hemodialysis, with only 12% utilizing home dialysis options including peritoneal dialysis. Clinical challenges and patient outcomes Late referrals remain a significant challenge, with 44% of patients requiring catheters at their first dialysis session according to the 2023 dialysis registry. Infection remains a leading cause of death among dialysis patients, followed by cardiovascular disease at 24%. Patients with end-stage kidney disease represent a high-risk group, with CKD ranked as the 16th leading cause of death in 2016. Projections indicate that by 2040, CKD could rise to become the fifth leading cause of death, highlighting the urgent need for improved quality of care and early intervention strategies. |
EXPLORE FURTHER
The silent crisis: Examining acute kidney injuryKey symptoms to identify for early detection of acute kidney injury
|
Pros and cons of getting a kidney transplantOnly half of dialysis patients survive five years post-treatment
|
Early warning signs of kidney cancerTumors often discovered incidentally; symptoms include painless haematuria and swelling
|
Nephrologist says only 30 get into kidney donation programme from 21,000 in waiting listThe average waiting time for an organ transplant is between 14 and 16 years
|
Renal denervation consensus paper now published in hypertension research journalA collaborative effort to combat hypertension
|
National Kidney Foundation refutes claims of viral posting promoting a cure for kidney disease
Jisheng Kidney Qi tablets - a cure for kidney disease a scam, says NKF
|
Cranberries, high doses of vitamin C causes kidney stones, says clinical journalOxalate in cranberries a contributing factor
|
Mybuahpinggang.com website launched to empower kidney failure patients, caregivers nationwidePractical resources on kidney diseases, treatment, dialysis and transplant
|